Genetic Factors Behind Lymphedema Risk: Understanding Hereditary Causes and Management
Primary lymphedema arises from inherited anomalies in lymphatic vessel development, creating a lifelong predisposition to fluid accumulation and tissue swelling. By exploring genetic predisposition to lymphedema, we uncover how specific gene mutations, inheritance patterns, diagnostic techniques, and targeted rehabilitation services converge to improve patient outcomes. This guide examines seven key themes: lymphedema therapy
- The distinction between primary and secondary lymphedema
- Core genetic mutations and inheritance
- Diagnostic strategies and genetic testing
- Classification of hereditary lymphedema subtypes
- Specialized rehabilitation approaches
- Patient experiences and support networks
- Emerging research and personalized medicine
With compassionate expertise and practical insights, we empower individuals and families to navigate lymphedema therapy risk and management.
What Is Primary Lymphedema and How Does It Differ from Secondary Lymphedema?
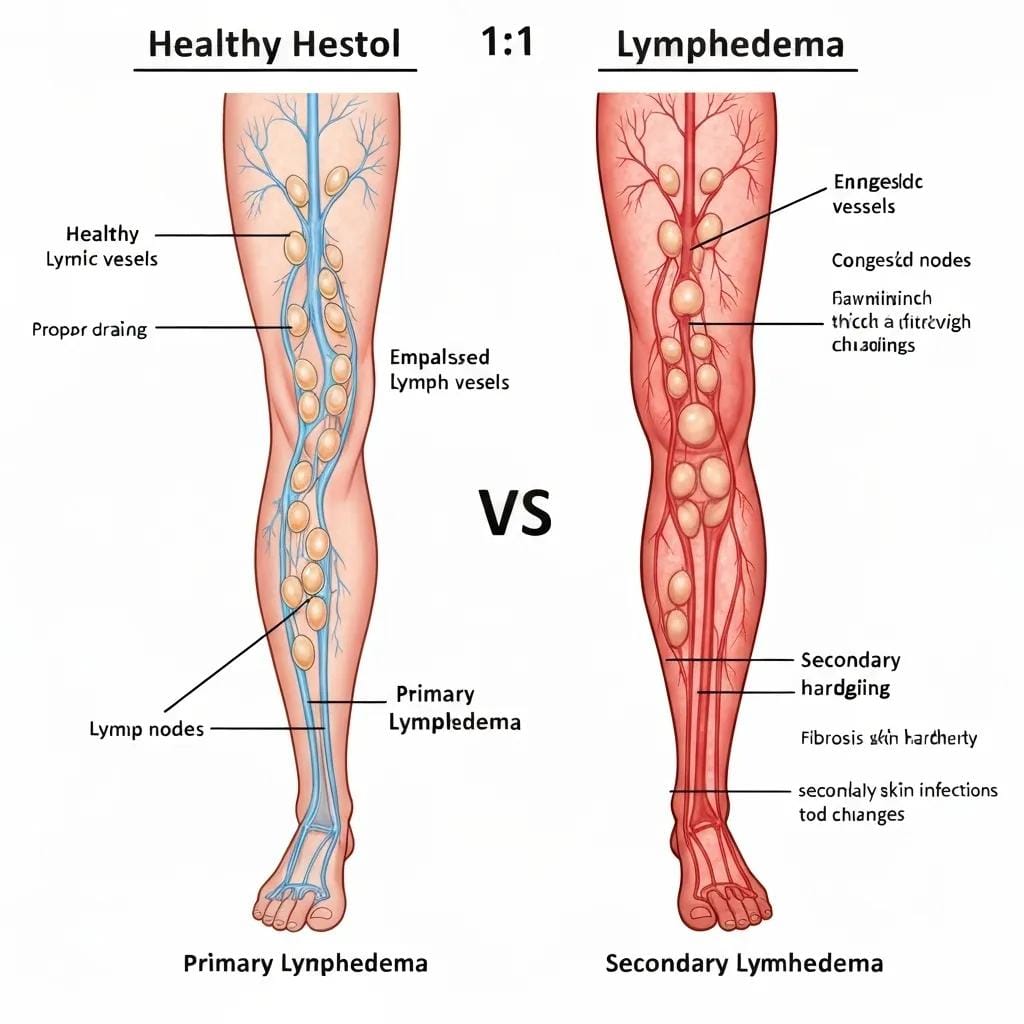
Primary lymphedema is a congenital or hereditary condition resulting from genetic mutations that impair lymphatic vessel formation and function. This contrasts with secondary lymphedema, which develops after lymphatic damage due to trauma, infection, surgery, or radiation therapy. lymphedema therapy
Primary Lymphedema: Update on Genetic Basis and Management
Primary lymphedema is a chronic condition resulting from errors in lymphatic development, with genetic causes identified in a subset of patients. This review highlights that while most cases are sporadic, over 20 genes are known to contribute to primary lymphedema, including those associated with Milroy disease (VEGFR3) and lymphedema-distichiasis syndrome (FOXC2).
This research provides a comprehensive overview of the genetic underpinnings of primary lymphedema, supporting the article’s distinction between primary and secondary forms and the role of various gene mutations.
What Are the Key Characteristics of Primary Lymphedema?
- Onset timeline: Present at birth (congenital) or emerging during puberty or adulthood
- Genetic origin: Caused by mutations in lymphatic development genes
- Chronic progression: Gradual swelling and tissue changes without an external injury trigger
These characteristics establish the foundation for hereditary risk evaluation and guide personalized rehabilitative interventions.
How Is Primary Lymphedema Different from Secondary Lymphedema?
Primary lymphedema arises from intrinsic genetic defects, whereas secondary lymphedema results from acquired lymphatic injury. In primary forms, family history often reveals similar cases, while in secondary lymphedema, onset typically follows surgery (e.g., cancer lymph node removal) or infection (e.g., filariasis).
What Are the Common Symptoms and Signs of Primary Lymphedema?
- Persistent limb swelling, often asymmetric
- Sensation of heaviness or tightness in affected areas
- Recurrent skin infections such as cellulitis
- Skin changes including fibrosis, hyperkeratosis, or warty overgrowth
Recognizing these signs early enables prompt genetic evaluation and initiation of tailored lymphedema therapy.
Which Genetic Mutations Cause Primary Lymphedema?
Primary lymphedema is caused by mutations in genes essential for lymphatic vessel growth, valve formation, and vessel integrity. Understanding these genetic predisposition to lymphedema genes directs diagnosis and informs rehabilitation planning.
- FLT4 (VEGFR3) – Milroy Disease
- FOXC2 – Meige Disease and Lymphedema-Distichiasis
- GATA2 – Emberger Syndrome
- PIK3CA – CLOVES and lymphatic channel anomalies
- SOX18 – Hypotrichosis–Lymphedema–Telangiectasia
- CCBE1 – Hennekam Syndrome
This list of genes highlights inherited mutation targets essential for comprehensive genetic screening.
What Role Does the FLT4 Gene Play in Milroy Disease?
The FLT4 gene encodes VEGFR-3, a receptor critical for lymphatic endothelial cell growth and valve development. Mutations in FLT4 lead to Milroy Disease, a congenital lymphedema appearing at or shortly after birth. Impaired VEGFR-3 signaling disrupts normal vessel formation, causing lifelong fluid retention in lower limbs.
FLT4 Mutations Are Associated with Segmental Lymphatic Dysfunction and Initial Lymphatic Aplasia in Patients with Milroy Disease
A study exploring mutations in the FLT4 gene (VEGFR3) in patients with Milroy disease identified 28 variants, with 16 being novel. The findings indicate that segmental dysfunction of lymphatic vessels and initial lymphatic aplasia are present in Milroy disease patients with FLT4 mutations, contributing to congenital lower limb swelling.
This study directly supports the article’s discussion on the FLT4 gene’s role in Milroy Disease, detailing its genetic basis and impact on lymphatic vessel formation.
How Does the FOXC2 Gene Affect Meige Disease and Lymphedema-Distichiasis?
The FOXC2 gene regulates transcription factors that guide lymphatic valve morphogenesis. FOXC2 mutations produce Meige Disease (lymphedema praecox) between ages 9 and 25, and Lymphedema-Distichiasis Syndrome, characterized by extra eyelashes. Aberrant valve formation promotes retrograde lymph flow, leading to progressive swelling.
What Other Genes Are Linked to Hereditary Lymphedema?
Beyond FLT4 and FOXC2, several genes contribute to primary lymphedema:
- GATA2: Impacts immune cell and lymphatic development, associated with Emberger Syndrome
- PIK3CA: Influences cellular growth pathways, leading to vascular malformations and lymphatic channel dilation
- SOX18: Drives differentiation of lymphatic endothelial progenitors, linked to skin and hair abnormalities
- CCBE1: Facilitates lymphatic budding from veins, with mutations causing Hennekam Syndrome
Inheritance Patterns of Genetic Lymphedema
| Inheritance Pattern | Characteristic | Example Genes |
|---|---|---|
| Autosomal Dominant | Single mutated copy sufficient; vertical family transmission | FLT4, FOXC2, GATA2 |
| Autosomal Recessive | Two mutated copies required; siblings often affected | CCBE1, some PIK3CA variants |
How Is Genetic Lymphedema Diagnosed and What Is the Role of Genetic Testing?
Genetic lymphedema diagnosis combines clinical evaluation, family history, imaging, and molecular testing to confirm inherited mutations. Genetic testing pinpoints causative gene alterations, enabling targeted counseling and management recommendations.
Development and physiological functions of the lymphatic system: insights from human genetic studies of primary lymphedema
Genetic studies have been crucial in recognizing primary lymphedema as a heterogeneous condition with diverse genetic causes and disease mechanisms. This review discusses the biological functions of several genes vital for lymphatic system development and function, providing a basis for understanding normal lymphatic biology and the conditions arising from mutations in these genes.
This review article reinforces the importance of genetic studies in diagnosing and understanding primary lymphedema, aligning with the article’s focus on diagnostic strategies and genetic testing.
When Should Genetic Testing Be Considered for Lymphedema?
Genetic testing is appropriate when:
- Lymphedema presents before age 35 without an obvious cause
- Multiple family members exhibit limb swelling
- Syndromic features accompany swelling (e.g., distichiasis, hearing loss)
- Imaging shows hypoplastic or aplastic lymphatic channels
What Does the Genetic Testing Process Involve?
Genetic testing for lymphedema typically follows these steps:
- Pre-test Counseling – Discussion of risks, benefits, and implications
- Sample Collection – Blood or saliva sent to specialized laboratories
- Gene Panel Analysis – Screening of known lymphedema genes
- Variant Interpretation – Expert review of mutations for clinical significance
This structured workflow ensures accurate identification of hereditary predisposition to lymphedema and aligns diagnostic information with rehabilitation strategies.
How Are Genetic Test Results Interpreted for Lymphedema?
- Pathogenic Variant: Confirms hereditary lymphedema and guides personalized care
- Variant of Uncertain Significance: Requires additional family studies and reanalysis
- Negative Result: Suggests non-genetic or undiscovered gene causes; management remains symptom-driven
What Is Genetic Counseling and How Does It Support Patients?
Genetic counseling provides education and psychological support around hereditary lymphedema risk. Counselors explain inheritance patterns, test implications, family planning options, and refer individuals for specialized rehabilitation at rhw-indy.com to address functional and wellness needs.
What Are the Types of Genetically-Linked Primary Lymphedema?
Primary lymphedema subtypes are classified by age of onset, genetic cause, and associated clinical features. Recognizing these types aids in accurate diagnosis and targeted management.
| Lymphedema Type | Onset Age | Associated Gene | Key Feature |
|---|---|---|---|
| Milroy Disease | Birth – 2 years | FLT4 | Congenital lower limb swelling |
| Meige Disease | 9 – 25 years | FOXC2 | Early-adult swelling, distichiasis |
| Lymphedema Tarda | After 35 years | Various | Late-onset hereditary swelling |
| Syndromic Forms | Variable | GATA2, SOX18 | Multisystem involvement |
What Is Milroy Disease and Its Genetic Basis?
Milroy Disease is a congenital form of primary lymphedema caused by FLT4 mutations. Affected infants exhibit bilateral lower extremity swelling at birth with risk of cellulitis. Early diagnosis permits prompt intervention with manual lymph drainage and compression to delay fibrosis.
What Is Meige Disease (Lymphedema Praecox) and Its Genetic Causes?
Meige Disease manifests in adolescence or early adulthood and results from FOXC2 mutations. Patients often develop swelling in lower limbs accompanied by distichiasis (extra eyelashes). Targeted valve-support therapies and genetic counseling help manage progression and inform family risk.
What Is Lymphedema Tarda and How Is It Related to Genetics?
Lymphedema Tarda appears after age 35 without overt vessel damage. Although inheritance patterns can be unclear, genetic predisposition is implicated in disrupted lymphatic maintenance genes. Recognizing this late-onset form ensures lymphedema therapy even in adults.
How Do Syndromic Forms of Lymphedema Relate to Genetic Mutations?
Certain syndromes combine lymphedema with other anomalies:
- Noonan Syndrome (PTPN11) – cardiac defects + lymphatic dysplasia
- Klippel-Trenaunay Syndrome (PIK3CA) – vascular malformations + limb overgrowth
- Hennekam Syndrome (CCBE1) – facial anomalies + intestinal lymphangiectasia
How Can Genetically-Linked Lymphedema Be Managed Through Rehabilitation?
Effective rehabilitation for hereditary lymphedema centers on reducing swelling, preserving function, and preventing complications through specialized therapies tailored to genetic subtypes.
Specialized rehabilitation services blend evidence-based techniques with genetic insights to optimize outcomes for primary lymphedema.
What Specialized Rehabilitation Services Are Available for Primary Lymphedema?

Comprehensive care programs include:
- Manual lymph drainage performed by certified therapists
- Custom-fitted compression garments to maintain reduced limb volume
- Therapeutic exercise to enhance lymphatic flow and muscle strength
- Skin and nail care education to prevent infection
How Does Complete Decongestive Therapy (CDT) Help Manage Genetic Lymphedema?
Complete Decongestive Therapy combines four synergistic components:
- Manual Lymph Drainage to mobilize fluid
- Compression Bandaging to support tissue and prevent refilling
- Exercise Regimens to activate lymphatic pumps
- Skin Care to minimize infection risk
Predictors of the Efficacy of Lymphedema Decongestive Therapy
Complete Decongestive Therapy (CDT) is recognized as the primary treatment for lymphedema, combining manual lymphatic drainage, compression bandaging, skincare, and exercise. Early diagnosis and initiation of CDT are critical for preventing irreversible damage and worsening symptoms, with successful outcomes depending on timely treatment and patient adherence.
This research supports the article’s section on specialized rehabilitation approaches, particularly the effectiveness and components of Complete Decongestive Therapy in managing lymphedema.
What Are Pediatric Management Strategies for Congenital Lymphedema?
Pediatric approaches address growth and development:
- Gentle manual drainage and playful exercises to engage children
- Lightweight compression garments designed for comfort and compliance
- Family education on infection prevention and daily limb inspection
How Can Patients Practice Long-Term Self-Management and Care?
Long-term self-care involves:
- Daily self-bandaging or compression sleeve application
- Regular limb measurement to track volume changes
- Incorporating skin hygiene practices and infection monitoring
- Staying active with lymphatic-friendly exercises like swimming or cycling
What Are Patient Experiences and Support Resources for Genetic Lymphedema?
Personal narratives and community connections provide hope, practical tips, and emotional support for those navigating hereditary lymphedema.
How Do Patient Stories Illustrate Living with Genetic Lymphedema?
Individual experiences highlight resilience and adaptation:
- A young adult with Milroy Disease who found relief through early CDT
- A teenager with Meige Disease balancing school activities with compression therapy
- A late-onset patient whose genetic diagnosis enabled targeted monitoring
What Support Resources Are Available for Families and Patients?
Families and individuals can access:
- Patient advocacy groups offering peer mentorship
- Online forums dedicated to lymphedema genetics education
- Local support networks coordinating group exercise and bandaging workshops
How Does Understanding Genetics Improve Patient Outcomes?
Knowledge of one’s genetic mutation guides proactive screening for complications, informs realistic expectations, and enhances collaboration with rehabilitation specialists to design personalized care plans.
What Are the Latest Trends and Research in Genetic Lymphedema?
Advances in molecular science and therapeutic innovation are rapidly reshaping hereditary lymphedema care.
How Is Genetic Research Advancing Lymphedema Diagnosis and Treatment?
Cutting-edge studies employ next-generation sequencing to uncover novel mutations, while gene editing models explore targeted therapies to restore lymphatic function at a molecular level.
What Are Emerging Genetic Markers and Their Clinical Implications?
Novel markers such as isoform-specific PIK3CA variants and noncoding region mutations expand diagnostic accuracy and reveal pathways for pharmaceutical interventions aimed at lymphangiogenesis.
How Is Personalized Medicine Shaping Future Lymphedema Care?
Integrating genomic profiles with wearable sensor data enables real-time monitoring of limb volume changes, supporting adaptive compression protocols and early intervention algorithms to prevent disease progression.
Living with hereditary lymphedema demands ongoing commitment to specialized therapies, self-management practices, and community engagement. By combining genetic insights with tailored rehabilitation services and compassionate support at rhw-indy.com, patients can achieve sustained mobility, reduced swelling, and an improved quality of life. Reach out for a personalized assessment and discover how our team of experts can help you navigate genetic lymphedema with confidence and care.
Frequently Asked Questions
What lifestyle changes can help manage primary lymphedema symptoms?
Managing primary lymphedema often involves adopting specific lifestyle changes. Regular physical activity, such as swimming or walking, can enhance lymphatic flow and reduce swelling. Maintaining a healthy diet rich in antioxidants and low in sodium can also help manage fluid retention. Additionally, practicing good skin care to prevent infections and wearing compression garments as recommended by healthcare providers are crucial. Staying hydrated and avoiding prolonged periods of inactivity can further support lymphatic health and improve overall well-being.
Are there any surgical options for treating hereditary lymphedema?
Surgical options for hereditary lymphedema may be considered when conservative treatments are insufficient. Procedures such as lymphaticovenous anastomosis (LVA) or vascularized lymph node transfer (VLNT) aim to restore lymphatic drainage by connecting lymphatic vessels to veins or transplanting lymph nodes. These surgeries can help reduce swelling and improve limb function. However, candidacy for surgery depends on individual circumstances, including the severity of lymphedema and overall health, so a thorough evaluation by a specialist is essential.
How can genetic counseling assist families affected by lymphedema?
Genetic counseling plays a vital role for families affected by lymphedema by providing education about the hereditary nature of the condition. Counselors help families understand inheritance patterns, assess risks for future generations, and discuss the implications of genetic testing. They also offer emotional support and resources for coping with the challenges of living with lymphedema. By facilitating informed decision-making, genetic counseling empowers families to navigate their health and wellness proactively.
What role does early diagnosis play in managing lymphedema?
Early diagnosis of lymphedema is crucial for effective management and improved patient outcomes. Identifying the condition promptly allows for timely interventions, such as Complete Decongestive Therapy (CDT), which can significantly reduce swelling and prevent complications. Early treatment can also help patients develop self-management strategies and lifestyle modifications that enhance their quality of life. Additionally, understanding the genetic basis of lymphedema can guide personalized care plans and facilitate better long-term management.
What are the psychological impacts of living with hereditary lymphedema?
Living with hereditary lymphedema can have significant psychological impacts, including feelings of anxiety, depression, and social isolation. Patients may struggle with body image issues due to visible swelling and may feel self-conscious in social situations. Support groups and counseling can provide valuable emotional support, helping individuals share experiences and coping strategies. Engaging with a community of others facing similar challenges can foster resilience and improve mental well-being, making it an essential aspect of lymphedema therapy.
How can technology aid in the management of lymphedema?
Technology plays an increasingly important role in managing lymphedema. Wearable devices can monitor limb volume changes in real-time, allowing for timely adjustments in compression therapy. Mobile applications can help patients track symptoms, manage appointments, and access educational resources. Additionally, telehealth services enable patients to consult with specialists remotely, ensuring continuous support and guidance. These technological advancements enhance patient engagement and empower individuals to take an active role in their lymphedema management.